Type 2 diabetes can now be effectively treated and prevented using early, aggressive combination therapy, say the 82nd Scientific Sessions panelists for the Future of Diabetes—The Next Frontier with Dual Incretin, presented on Tuesday, June 7.
The emergence of incretin therapy has revolutionized the management of type 2 diabetes. Before the 1980s, it was not clear that improving glucose control could prevent or delay the development of diabetes complications. It wasn’t until the incretin effect was documented in 1982 that there was a glimmer of hope that type 2 diabetes could be managed effectively.
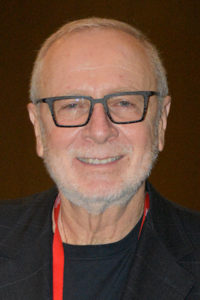
“A1C should no longer be the trigger for combination therapy,” said Julio Rosenstock, MD, Director, Velocity Clinical Research at Medical City and Clinical Professor of Medicine at University of Texas Southwest Medical Center. “Combination therapy should be the preferred first-line approach regardless of A1C. We are in a position to move the goalpost to remission or reversal of type 2 diabetes.”

Dr. Rosenstock was among the experts who discussed the future of dual incretin therapy. The session was livestreamed and can be viewed on-demand by registered meeting participants at ADA2022.org. If you haven’t registered for the 82nd Scientific Sessions, register today to access the valuable meeting content.
“There was only sulfonylureas and insulin for type 2 diabetes for years,” said Rodolfo J. Galindo, MD, FACE, Associate Professor of Medicine, Emory University. “Before the first incretin in 2005, we were slowly closing the gap with the discovery of GIP (glucose-dependent insulinotropic polypeptide), GLP-1 (glucagon-like peptide-1), DPP-IV (dipeptidyl peptidase IV), and finally, exenatide. Now we have the first dual GIP/GLP-1 receptor agonist, tirzepatide.”
As type 2 diabetes medications have become more effective, management goals have become more ambitious, Dr. Galindo said. It is no longer enough to lower A1C. The ideal type 2 diabetes medication can control glycemia with low risk of hypoglycemia and produce beneficial effects on beta cell function, weight loss, and cardiorenal function.
Tirzepatide meets all the criteria, he added, and is just a first step. At least 20 other novel incretins are in development with the promise of improved control of weight and other factors critical in type 2 diabetes.

“Weight and considerations of weight management factor into our treatment decisions and plans at many points,” said Jennifer B. Green, MD, Professor of Medicine, Duke University Medical Center. “Weight loss is a huge component of diabetes management and is not easy to accomplish with our traditional tools. Most people need to maintain at least a 5% weight loss to show improvement in A1C. The more the weight loss, the more the decline in A1C.”
The ADA 2022 standard of care for type 2 diabetes recommends ≥5% weight loss for most people with the disease. Dual GIP/GLP-1 agents are the most effective weight loss agents developed so far in diabetes, Dr. Green noted. The SURPASS trials, which supported the approval of tirzepatide, demonstrated weight loss greater than 30% of initial body weight and A1C ≤5.7% in significant numbers of participants. Across all the SURPASS trials, 40-50% of participants achieved normoglycemia and significant weight loss without hypoglycemia.
Dual receptor agonism is both additive and complementary, Dr. Green explained. GLP-1 activity reduces food intake, improves insulin secretion, reduces glucagon secretion, and delays gastric emptying. GIP activity also reduces food intake and improves beta cell function while improving insulin sensitivity and nutrient metabolism.
Dual incretin receptor agonism also brings important renal benefits and, at a minimum, carries no increased cardiovascular risk. Cardiovascular benefits are still in trial. The renal benefits alone are a dramatic improvement over existing management options.

“Proportionally, there are more people with diabetes in the nephrology clinic than in the endocrine clinic,” said Katherine R. Tuttle, MD, FACP, FASN, FNKF, Executive Director for Research, Providence Health Care, and Professor of Medicine, University of Washington Institute of Translational Health Sciences.
People with diabetic kidney disease (DKD) are an important population because chronic kidney disease (CKD) amplifies cardiovascular disease (CVD) risk and most CVD risk associated with diabetes occurs in individuals with CKD, she explained.
Only 10% of those with DKD progress to end-stage kidney disease, Dr. Tuttle continued. Of the 90%, half die from CVD and a third from infection, including COVID-19. With dual GIP/GLP-1 receptor agonism, DKD is a modifiable condition.
GLP-1 agents alone demonstrate potent cardiovascular protection irrespective of baseline kidney function, Dr. Tuttle said. SURPASS showed that dual agonism has potent renal protection with a hazard ratio of 0.41 for albuminuria versus insulin glargine and 0.87 for eGFR decline. The effects of tirzepatide were independent of sodium-glucose cotransporter-2 (SGLT2) inhibitor use.
“We know it is safe to give them together, and they are likely working in a complementary fashion. We have good rationale for combination therapy with GIP/GLP-1 and SGLT2 agents,” Dr. Tuttle said.
Cancer clinicians long ago recognized that aggressive early treatment followed by maintenance therapy is more successful than step therapy, Dr. Rosenstock explained. The same rationale applies to type 2 diabetes.
“We need to focus on combination therapy from day one in type 2 diabetes,” he said. “If we continue doing sequential therapy, we are not going to improve our results.”
High-dose semaglutide can bring significant numbers of people to A1C ≤6.5%, he noted. SURPASS brought nearly all participants to ≤6.0% and over half to ≤5.7%. Tirzepatide also produced ≥15% weight loss in up to 43% of participants. And of all SURPASS participants who had prediabetes, 95% returned to normoglycemia.
“There is real potential to get back to normal,” Dr. Rosenstock said. “Reversal of type 2 diabetes has always been a dream. Tirzepatide has moved the goalpost to attaining diabetes reversal or remission.”
“We have a very powerful tool to get to normoglycemia,” he added.
[sub-post-content]