
Two researchers went head-to-head in a virtual debate examining whether artificial pancreas systems should be single hormone (insulin only) or dual hormone (insulin and glucagon or dasiglucagon) during the Virtual 80th Scientific Sessions.
The Current Issues debate Should the Artificial Pancreas Be Single or Dual Hormone? can be viewed by registered meeting attendees at ADA2020.org through September 10, 2020. If you haven’t registered for the Virtual 80th Scientific Sessions, register today to access all of the valuable meeting content.
Roman Hovorka, PhD, FMedSci, made the case for a single-hormone artificial pancreas system, arguing it’s more efficient and cost effective. Steven J. Russell, MD, PhD, presented a counterargument in favor of a dual-hormone system.
Dr. Hovorka said two principles make for a good artificial pancreas system—good glucose control (about 70% time-in-range) and low burden on the patient (11 to 20 minutes of use per day). The Tandem-Control IQ pivotal trial published last year in The New England Journal of Medicine showed that the t:slim X2™ insulin pump with Control-IQ™ technology, a single-hormone, closed-loop system, improved time-in-range by about 11%, reduced mean glucose by 0.7mmol/l, reduced time-in-hypoglycemia by 1%, and reduced A1C by 0.3% over six months compared to a control group using pump therapy alone, he reported.
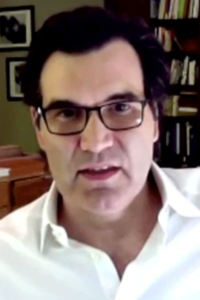
“Those are good glucose values,” said Dr. Hovorka, Professor of Metabolic Technology in the Department of Pediatrics at the University of Cambridge, United Kingdom. “The time-in-range benefits are better in the overnight period. The benefits are also achieved quickly—within one to four weeks—and the improvement was sustained over the six months of the study.”
The U.S. Food and Drug Administration first approved automated insulin delivery devices for type 1 diabetes in 2016. Four years later, there are several companies producing insulin-only, closed-loop systems: Tandem, Tidepool, Omniod, and Beta Bionics in the U.S., and CamDiab in the European Union.
In the month prior to his presentation, Dr. Hovorka reported that of 160 subjects ages 2 to 80 years using the CamAPS® FX closed-loop system by CamDiab, 7% of users had a time-in-range of 90% or greater; 28% had time-in-range of 80% or greater; 69% had time-in-range of 70% or greater; and 87% of users had time-in-range of 60% or better.
Dr. Hovorka also shared averages from multiple studies examining the time burden of the CamDiab system. Newly diagnosed teenagers spent roughly 10 minutes per day using the system while teenagers overall spent 17 minutes per day using the system on average; adults spent 17 minutes per day on average; pregnant women spent 33 minutes on average; adults 60 years and older spent 67 minutes on average; and parents of young children spent 81 minutes on average.
“Insulin-only, closed-loop systems are suitable for the majority of people with type 1 diabetes,” Dr. Hovorka said. “While the dual-hormone field is catching up, the insulin-only field is not standing still—faster insulins, advanced algorithms, regulatory and reimbursement pathways, and cost pressure by payers. The dual-hormone system will need to catch up with these developments.”
There are some ongoing challenges with single-hormone systems, Dr. Hovorka admitted, including exercise-related dysglycemia, missed boluses, and delayed insulin absorption. However, dual-hormone delivery does not accelerate insulin absorption, he noted.
Dr. Russell, Associate Professor of Medicine at Harvard Medical School and Associate Physician at Massachusetts General Hospital, said a bi-hormonal system has the potential to achieve lower glucose, longer time-in-range, and less hypoglycemia than a well-functioning insulin-only system. In a meta-analysis of both single- and dual-hormone systems, the single-hormone system increased time-in-range by 11% while the dual system increased it by 19.52%, nearly twice as much, he noted. In addition, the single-hormone system reduced time-in-hypoglycemia by 1.9% while the dual system reduced it by 3.78%.
“Imagine a scenario where blood glucose is in the normal range—close to the bottom, which is often the case with a good artificial pancreas system—and something changes. For instance, the person starts to exercise and they have glucose uptake out of their blood and into their muscle,” Dr. Russell said. “They can drop into the hypoglycemic range very rapidly. Because insulin is absorbed relatively slowly, even if you stop giving insulin at this point, you’re not going to be able to prevent that hypoglycemic event. You’re going to have to take medicinal carbohydrates. Alternatively, the system can automatically give you glucagon, which can prevent the low from happening. If you have a bi-hormonal system, that can happen without the user taking action.”
One of the biggest concerns with a dual-hormone system is that the second drug adds costs, both researchers noted, but Dr. Russell justified the cost.
“This system can be manufactured in such a way that it doesn’t have to be more expensive and yet it adds substantial value,” he said. “The addition of glucagon would be justified by the improved outcomes, improved quality of life, and the ability to be more spontaneous around exercise that comes with having automated prevention and treatment of hypoglycemia.”
VIEW THIS PRESENTATION
Already registered?
View this presentation at ADA2020.org
Not yet registered?
Register now to access all presentations from the Virtual 80th Scientific Sessions