New estimates published during the Scientific Sessions in The Lancet from the Institute for Health Metrics and Evaluation (IHME) indicate that more than 1.31 billion people worldwide could be living with diabetes by 2050. The increase in prevalence, up from 529 million in 2021, is expected to be driven by increases in type 2 diabetes.

The Joint ADA/The Lancet Symposium—Global Inequity in Diabetes—An International Perspective brought together a panel of health experts from Australia, India, and the United States to discuss the global health inequity of diabetes and launched a three-paper series on the topic in The Lancet and The Lancet Diabetes & Endocrinology. The symposium can be viewed on-demand by registered meeting participants at ADA2023.org. If you haven’t registered for the 83rd Scientific Sessions, register today to access the valuable meeting content through August 28.
One paper in the series looks at the role of structural racism and geographic inequity in diabetes outcomes. Researchers Louise J. Maple-Brown, MBBS, FRACP, PhD, and Sian Graham, BAppSc, Menzies School of Health Research, Charles Darwin University, Australia, presented their theoretical framework and five social determinants of health (SDOH), which were selected because of their impact on diabetes outcomes.

The SDOH include economic development, public awareness and policy, access to high-quality care, innovations in diabetes management, and sociocultural norms.
One framework showed minority groups starting off with a disadvantage that increases with the influence of downstream SDOH.
“The compound effects of structural inequity and SDOH across multiple generations fuel a cascade of ever-widening global inequity in diabetes,” Dr. Maple-Brown said.
Ms. Graham brought a First Nations, aboriginal perspective to the panel. She described the intergenerational effects of diabetes in her own family and how it normalized the disease. She has been determined to work to prevent the next generation, including her own daughters, from walking the same path.

Saria Hassan, MD, MPH, Assistant Professor of Medicine at Emory University School of Medicine and Department of Global Health, Rollins School of Public Health, discussed another paper in the series that deals with disparities in diabetes prevalence and management by race and ethnicity in the U.S., and how to improve.
She discussed the multidimensional reality of diabetes disparities in the U.S., with a focus on geographic variability as well as inter- and transgenerational changes. Notably, Native American populations have a significantly higher prevalence of diabetes than any other race or ethnicity.

Her proposed paths moving forward include actions that can be taken by researchers, funders of research, health administrators and practitioners, and policymakers.
“These disparities don’t exist because we don’t know how to fix the problem,” she said. “It’s more so that we have not translated the evidence into practice and policy equitably, and we have the tools to do that.”
Shivani Agarwal, MD, MPH, Associate Professor in the Department of Medicine at Albert Einstein College of Medicine, and Ashby F. Walker, PhD, Director of Health Equity Initiatives, University of Florida Diabetes Institute, co-presented on the last paper in The Lancet series, focusing on real-world international case studies to address global inequality in diabetes.

Drs. Agarwal and Walker outlined conceptual frameworks to show how the global crisis of diabetes is accelerating and being fueled by inequity, but said tangible solutions exist to counteract this.
“We cannot simply focus on individual-level solutions,” Dr. Walker said. “We must approach the individual within a larger social and structural context.”
One of the areas that need a paradigm shift is medical education, and then health care systems need to incorporate unmet social needs into diabetes care, they said. Policymakers must become versed in appropriate, equitable funding and programs, and they must remember that community is the key.
“Stakeholders and local knowledge must be valued and incorporated from inception to delivery to evaluation to sustainability of every program,” Dr. Agarwal said.
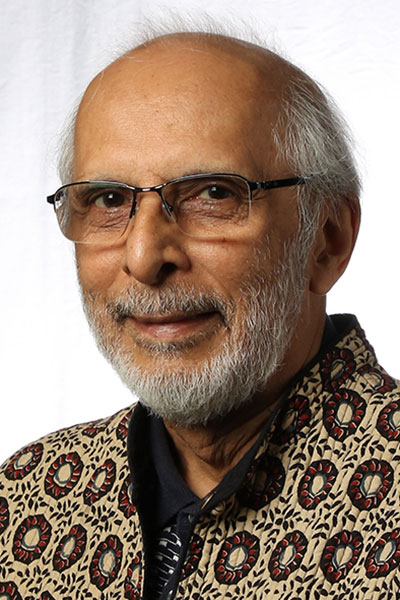
The presenters were joined on stage by panelists Chittaranjan Yajnik, MD, FRCP, Director of the Diabetes Unit at King Edward Memorial Hospital Research Centre, and Usha Sriram, MBBS, Director of the Department of Diabetes and Endocrinology at Voluntary Health Services, both in India.
Dr. Yajnik offered insight into the intergenerational factor of diabetes inequity with an example of maternal nutrition even before conception that affected diabetes outcome for babies.
“Women’s health is a nation’s wealth,” Dr. Yajnik said. “If you improve the health of women, across the life course there are big benefits.”