Experts in the field of diabetes and technology participated in a panel discussion on what diabetes quality teams can learn from engineers and designers, and how that knowledge can be translated into better understanding for end users, whether they be clinician or patients.
What Can Diabetes Quality Teams Learn from Engineers and Designers? can be viewed by registered meeting participants at ADA2023.org. If you haven’t registered for the 83rd Scientific Sessions, register today to access the valuable meeting content through August 28.
Panelists fielded questions from the audience as they shared their experiences with engineering and design processes and their contributions to the objective of improving the quality of care for people with type 1 and type 2 diabetes.

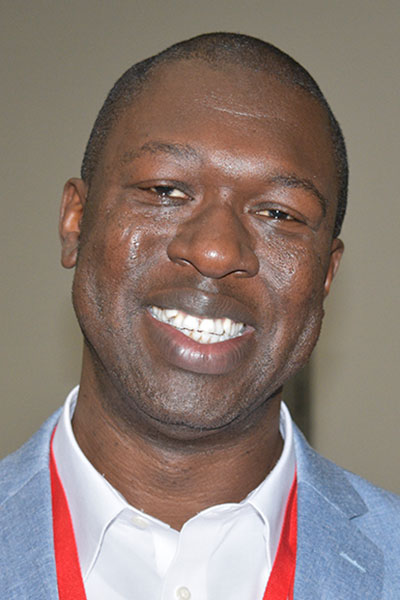
Speakers included Osagie Ebekozien, MD, MPH, CPHQ, Chief Medical Officer for T1D Exchange, where he directs the Diabetes Quality Improvement network of 55 U.S. diabetes centers; Wendy Rogers, PhD, Khan Professor of Applied Health Sciences at the University of Illinois Urbana-Champaign and Director of the Health Technology Education Program; and Schafer C. Boeder, MD, researcher and Assistant Professor of Endocrinology and Metabolism at the University of California, San Diego.
Dr. Rogers outlined a framework for designing technology that supports patient self-care throughout the stages of illness, from diagnosis to planning and implementation to sustaining that self-care.
“It’s really a journey that we want to think about, from the patient side of things,” she said. “And I might design a different tool for providers.”
Dr. Rogers explained that the framework she presented could also apply to health-care providers, with different requirements because they need a different level of information than patients.
Dr. Boeder outlined the various stakeholders of such a framework, noting it is essential to know who you are designing for before a project begins.
“Stakeholders can be an individual or group who will affect or be affected by your project, and what their motivations are,” he said.
This involves both people who are supportive and those who can be barriers.
Dr. Ebekozien built on that topic by presenting information his group gathered for a study in the ADA journal Diabetes Spectrum outlining steps to improving the quality of initiatives in diabetes research and care in ways that advance equity and improve outcomes for everyone.
“A stakeholder is someone who contributes to the outcome,” he said. “We look at how to get all those stakeholder voices into that space.”
Dr. Ebekozien stressed that data is an important tool in quality improvement, and he offered examples from studies that showed how it can be used to improve quality and reduce inequity in diabetes outcomes.
“In our journey as quality teams, we can’t undermine the power of data, not just in describing the problem, but in finding solutions,” he said.

Design is a process, and knowing your users is an essential part of that process, Dr. Rogers said. Knowing the user—whether it’s patients or clinicians—must happen first, before even defining the problem, generating ideas, building prototypes, testing, and implementation.
Data is one of the sources for that user knowledge, Dr. Ebekozien said, and it can guide design and implementation with clarity.
“Once you have the insight that comes from data, sometimes the problems become glaringly obvious,” he said.
Qualitative data is equally important, Dr. Boeder said, and simply listening provides valuable insight and a great starting point.
“Whether you’re listening to providers or patients and family members, you’ll start to hear the issues they’re dealing with,” he said. “That can spark ideas and questions, and that is a good time to go look for data.”