Glycemic targets for hospitalized patients have been part of clinical practice since studies in the late 1990s demonstrated significant reductions in mortality with intensive insulin therapy in critically ill patients. Current guidelines generally recommend 140-180 mg/dL for hospitalized patients with diabetes or hyperglycemia, with some recommendations ranging as low as 100 mg/dL and as high as 200 mg/dL for non-critically ill patients.

“The adverse effects of hyperglycemia are well known, including increased risk for infection, renal complications, cardiac arrhythmia, ICU-associated polyneuropathy, prolonged length of stay, and increased mortality,” said Mary T. Korytkowski, MD, Emeritus Professor of Endocrinology and Metabolism Medicine at the University of Pittsburgh. “The specific glycemic threshold for harm associated with hyperglycemia has not been well-defined, but evidence suggests it is somewhere between 150 and 180 mg/dL. The harm threshold for hypoglycemia is blood glucose below 70 mg/dL.”
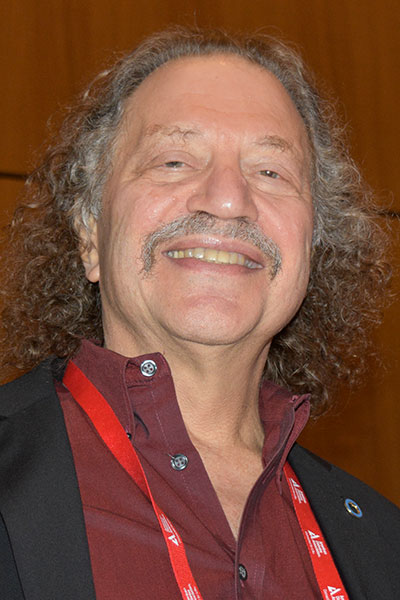
Dr. Korytkowski opened the Joint ADA/AACC Symposium Hyperglycemia in the Hospital—Are Our Tools for Measurement Accurate Enough? The session can be viewed on-demand by registered meeting participants at ADA2023.org. If you haven’t registered for the 83rd Scientific Sessions, register today to access the valuable meeting content through August 28.
How best to measure and control glycemia in the hospital remains unclear, Dr. Korytkowski added. Most hospitals use central labs and/or point-of-care testing (POCT) with glucose meters. Continuous glucose monitoring (CGM) has been shown to improve glycemic control while reducing the risk for hypoglycemia in outpatient settings and has the potential to promote safe, goal-directed glycemic management in hospitalized patients.
“Blood glucose meter measurements absolutely have to be accurate,” said David B. Sacks, MB, ChB, Senior Investigator, National Institutes of Health Department of Laboratory Medicine. “Hospitals use meter readings to adjust insulin doses and to avoid hypoglycemia.”
ADA guidelines recommend analytical imprecision of less than or equal to 2.9% and a bias of less than or equal to 2.2% for glucose meters. A 2018 review of glucose meters and hospital central labs found that all labs met ADA accuracy criteria, while just five out of 21 meters tested met those same standards.
“Laboratories are much more accurate than meters, which is to be expected,” Dr. Sacks said. “The low sample volume with meters and quick turnaround time, which patients like, are a challenge to accuracy.”
Sources of meter reading errors can include operator problems with sample contamination; expired test strips; adverse environmental conditions such as heat, humidity, and altitude; incorrect calibration; interference by medications; and many more.
Blood glucose meters are particularly poor at detecting hypoglycemia. U.S. Food and Drug Administration (FDA) criteria call for readings within 12 mg/dL of laboratory values. Given a true glucose of 65mg/dL, acceptable meter results range from 54-77 mg/dL, with some results outside even this broad range.
The latest guidelines and recommendations for laboratory analysis in diabetes were published in Diabetes Care and Clinical Chemistry in July.
CGM is becoming standard of care in the outpatient setting. And while many hospitals adopted CGM during COVID-19 to reduce infection risk, the technology has not yet been approved for hospital use by the FDA.

“CGM remains investigational in the hospital, but patients who already have CGM at home can continue to use it in hospital when possible,” said Guido Freckmann, MD, Medical Director and General Manager, Institut für Diabetes-Technologie Forschungs- und Entwicklungsgesellschaft mbH an der Universität Ulm, Ulm, Germany. He is also head of the International Federation of Clinical Chemistry and Laboratory Medicine Working Group on Continuous Glucose Monitoring.
“We learned from COVID that CGM in hospital is feasible, but there are challenges associated with staff training,” Dr. Freckmann added.
There are also potential problems with interfering substances and procedures. Multiple drugs can interfere with CGM accuracy, and no CGM is currently labeled to allow for exposure to radiologic imaging or therapy.
Surgical procedure can interfere with CGM readings if sensors are compressed by patient positioning. Electrocautery interference can disrupt CGM signaling, as can use of hypothermic devices.
“Accuracy has improved over the years and CGM systems reduce POCT but cannot replace it at this point,” Dr. Freckmann said. “We need more standardized metrics, procedures, and studies.”